How to prevent and treat the common long-distance running injury
The Illiotibial band, or ITB, is a thick fibrous non-contractile band originating from the top of the pelvis and running down to the outside of the leg and across the knee joint, connecting to the outside of the knee cap on its route. It passes over both the hip and the knee joint playing a role in stabilising both.
ITBS or Illiotibial Band Friction Syndrome is a common running injury, responsible for nearly one in 20 lower limb injuries in long-distance runners. According to research, at least 25% of all long-distance runners will experience it at some points in their lives – so it’s worth knowing a bit about it so you can be prepared.
- Amp up your training: How to get more from treadmill sessions
Exercise related pain is usually felt on the outside of the knee and around the Illiotibial Band. For runners this can be a continuous pain post session, but often can particularly noticeable when the foot hits the ground or when ascending or descending a gradient.
The traditional theory is that the ITB runs over the bone (femoral condyle) as the knee bends creating friction. Though this view has been challenged, with researchers saying there is a highly innervated fat between the bone and the ITB and it’s actually this that becomes inflamed as a result of ITB compression, thus causing the pain.
About the expert
Graham Burne is an extended scope, clinical specialist musculoskeletal and sports physiotherapist. He began his journey in musculoskeletal and sports physiotherapy by pursuing degrees in both physiotherapy and sports Science. He also has a strong personal background in strength and conditioning.
How are ITB issues caused?

There are many factors that can mean that runners are more likely to suffer from ITBS, however by far the most common two are:
Training error and changes in mileage
Training errors, usually due to overuse, are the most common contributing factor in the majority of running related injuries. Following a well progressed training programs allows the supporting structures of the pelvis and knee to adapt to increased stresses. Increasing the intensity, duration and frequency of the training runs, incorporating hills on the training routes too soon or even wearing incorrect footwear for your running style, may all overload the supporting structures of the knee, eventually leading to injury.
Muscle weakness at the hip abductors
The gluteal muscles provide stability at the hip and allow appropriate force transmission down the leg during stance and impact. The Gluteus medius (GM) acts to pull the knee outwards and stop it dropping in
If the Gluteus medius (especially the posterior fibres) is weak then another muscle, at the front of the hip (Tensor Fascia Latae) often becomes more active to compensate in providing hip stability. This muscle attaches to the ITB placing additional pressure on it. The result: As you continue to run, the Gluteus medius fatigues and the increased activity from Tensor Fascia Latae will cause the ITB to tighten up, compressing the outside of the knee.
How to prevent ITB Friction Syndrome?

One of the best ways to minimise the risk is to minimise hill training where possible. Consider training on level ground every other training day, and monitor for reoccurrence of symptoms, while gradually increasing distance and frequency.
Ensuring you have the right shoes for your foot type and running style is important for any runner, but more so if you’ve developed symptoms of ITBS. Choosing a shoe isn’t easy though, and there are many factors to take into consideration when there is a risk of injury. Many brands offer testing in store before purchase, and this will help to an extent. However the only way to really know if a shoe works for you is to test them out and monitor the effect they have on your running.
How to treat it
Firstly, you should monitor your running to find what triggers the pain to come on and keep notes on when and where it happens, whether that’s sprints, hill training or when you’ve hit a certain mileage. Once you have some insight into the cause, modify your training plan to account for that variable over a six to ten week period. If necessary a physio can help modify your training plan.
Proactive rest. This may seem simple but many runners struggle to incorporate enough into their training. If you’re showing signs of injury then it’s even more important to have longer rests, especially after long runs.
Effectively stretch the gluteal muscles, TFL and hip flexors if the ITBS is not too sore.
Gluteal strengthening and movement control exercises are often a good way to help treat ITBS, however not every ITB issue is caused by weak muscles. You should look into testing a training plan as it will help pinpoint if this is a primary cause of symptoms.
Exercises to prevent and treat
Side lying hip abduction in extension (posterior fibres)
How to do it: Lie on your side with affected leg above the other. With a controlled motion, lift the leg upwards as far as you can without causing pain and slowly lower back to the starting point.
Reps: 3 x 30

Side planks
How to do it: With your affected leg on the side closest to the floor, rest your arm under the shoulder and lift the hips until you reach a straight line across the whole body. Maintain that position for the full duration, or for as long as you can up until the time.
Reps: 5 x 30 second holds

Single leg Squats
How to do it: With your other leg placed firmly on the ground, lift the affected leg a few inches off the ground. Maintaining as upright a posture as possible, lower yourself to the ground in a controlled motion until you can’t go any further. Return slowly to the upright position.
Reps: 4 x 12

Single leg wall press (affected leg against wall)
How to do it: With your affected leg facing the wall, stand fully upright and lift the knee upwards. Press into the wall and maintain the hold.
Reps: 5 x 30 second holds

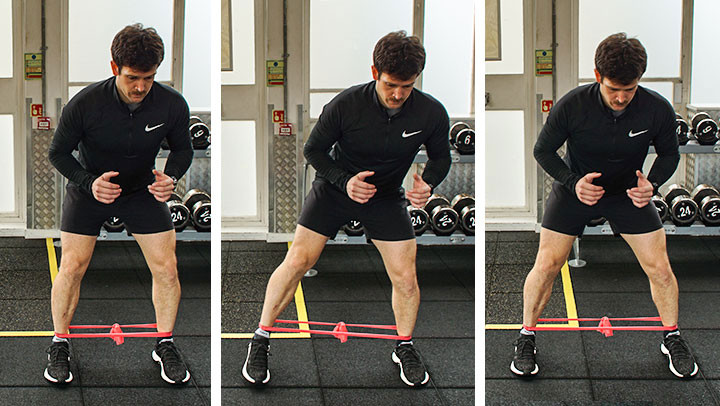
Banded abduction walks
How to do it: With your affected leg in the direction of movement and the resistance band placed between the ankles, make a slow and controlled step outwards. Land the foot fully on the ground and reset before repeating the process.
Reps: 5 x 20m walks
Complete 3x per week for a period of 12 weeks
Find out more
bmcmusculoskeletdisord.biomedcentral.com





