Treatment and prevention for this common and painful running injury
Anyone who’s suffered with plantar fasciitis will know how painful it can be, but for runners, it’s up there as one of the most debilitating reasons to put training on hold. Research has shown that it’s quite common as well, with the issue accounting for up to 10% of all running-related injuries.
The pain caused by plantar fasciitis, usually a stabbing sensation underneath the heel bone, can fluctuate depending on the type of activity and doesn’t necessarily happen during exercise itself. It’s classed as a degenerative condition due to the fact it’s commonly associated with the deterioration of collagen fibres and micro tears of the tissue.
- Amp up your training: How to get more from treadmill sessions
Scientifically speaking, the plantar fasciitis is a thick band of connective tissue which runs from the heel bone along the underside of the foot and attaches to the toes. Not only does it play an important role in maintaining the arch of the foot, but it’s also involved in absorbing forces during movement and contributes towards propelling us forward during walking and running. So for us runners, it’s a very important piece of biological kit.
About the expert
Patrick Carroll is a highly specialist Musculoskeletal Physiotherapist working within the NHS, sporting teams and for Wholelife Physiotherapy. After working in Melbourne, Australia as a strength and conditioning coach, Patrick completed his MSc (Pre-reg Physiotherapy) at the University of Essex.
How is it caused?

It’s not always clear why people develop plantar fasciitis as it affects both sedentary and active populations, but there is good evidence highlighting the risk factors for developing this condition.
Increased weight bearing activity can overload the plantar fascia tissue and trigger pain. This could be increasing running volume or even just switching to a job with more standing required. Being overweight also leads to changes in the structure of the plantar fascia and predisposes someone to developing issues.
Having a reduced arch of the foot or an excessive arch can also predispose to plantar fasciitis as it alters force dissipation through the plantar fascia. Excessively tight calf and soleus muscles can also affect plantar fascia function.
How to treat it

Educating people about this condition is essential to successful treatment. Understanding that it takes months rather than weeks to show significant signs of improvement, and also that advice about activity modification is central to good outcomes. Reducing activities that flare up the condition for a short period of time can also help pain levels settle.
Gradually building up activity levels again is also essential, rather than introducing large spikes of activity once there are initial signs of improvement. Footwear advice is important and cushioned supportive shoes with a gel heel insert can help reduce impact on the plantar fascia insertion, and also offload the connective tissue slightly by raising the heel.
In terms of active intervention, the traditional approach has been stretching the calf and soleus muscles as well as isolated stretching of the plantar fascia. More recent evidence recommends high load strength training of the calf, Achilles tendon and plantar fascia. This concept is borrowed from rehabilitating tendons, and early research is promising. The unique aspect of this strength training is that it puts high tensile stress through the plantar fascia by using the Windlass mechanism. This involves propping the big toe up during a heel raise, ultimately increasing the stress through the plantar fascia by more than 400% compared to stretching.
A ‘best practice’ rehabilitation plan should draw on the more traditional approach but also incorporate the newer strength-based approach.
Exercises to prevent and treat
Standing calf stretches
How to do it: With the balls of your affected foot standing on a raised platform and the heel lower, lift the heel with a controlled movement until you reach the highest point possible. Once done slowly lower back to the start position.
Reps: One minute of repetitions five times a day

Seated plantar fascia stretches
How to do it: Sitting on a raised platform or bench, place a weight onto the knee of the affected foot and raise the heel until the highest point possible. Slowly lower back to the starting position and repeat. The movement should take ten seconds to complete.
Reps: 10, twice daily

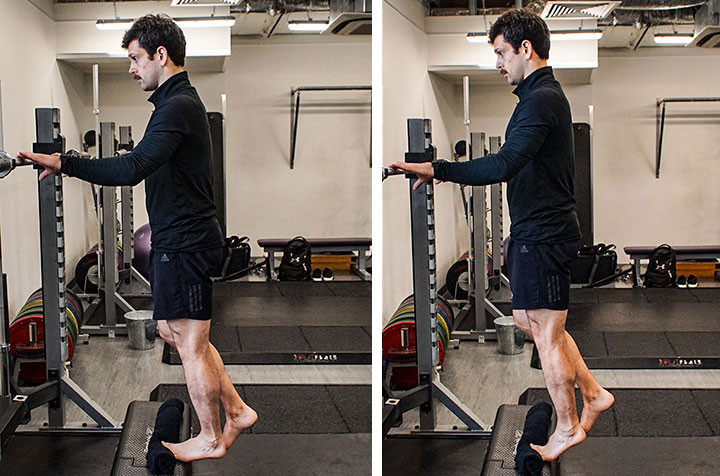
Single leg heel raises
How to do it: Stand on a raised platform with a towel elevating the big toe (to optimize the Windlass mechanism). Slowly lift the heel upwards until the highest point, then lower. Add external weight through a loaded backpack if the exercise is too easy.
Reps: 12, every other day
Note: In addition, aim to reduce weight-bearing activities for a two week period to allow symptoms to settle. For any weight-bearing activities use cushioned trainers with a gel heel insert.
Key References
DiGiovanni B et al (2003) “Tissue-specific plantar fascia-stretching exercise enhances outcomes in patients with chronic heel pain. A prospective, randomized study” The Journal of Bone & Joint Surgery (85) 1270–1277
Rathleef, M et al (2015) “High-load strength training improves outcome in patients with plantar fasciitis: A randomized controlled trial with 12-month follow-up: HL strength training and plantar fasciitis” Scandinavian Journal of Medicine and Science in Sports 25 (3) 292 – 300





